Integrated care is a term used to describe different models of health and social care delivery that aim to improve the coordination of care between different services and providers.
The main goals of integrated care are to:
- Improve the quality of care for patients/clients
- Reduce duplication of services and unnecessary costs
- Improve communication and coordination between different care providers
There are a variety of different models of integrated care, each with its own unique features. However, all models of integrated care share the same goal of improving the quality of care for patients/clients by reducing duplication of services and improving communication and coordination between different care providers.
This article provides an overview of what is meant by integrated care, the evidence that supports it as a health system model, the 5 key strategies needed to create a successful integrated care system, some examples from around the world, and their potential economic value.
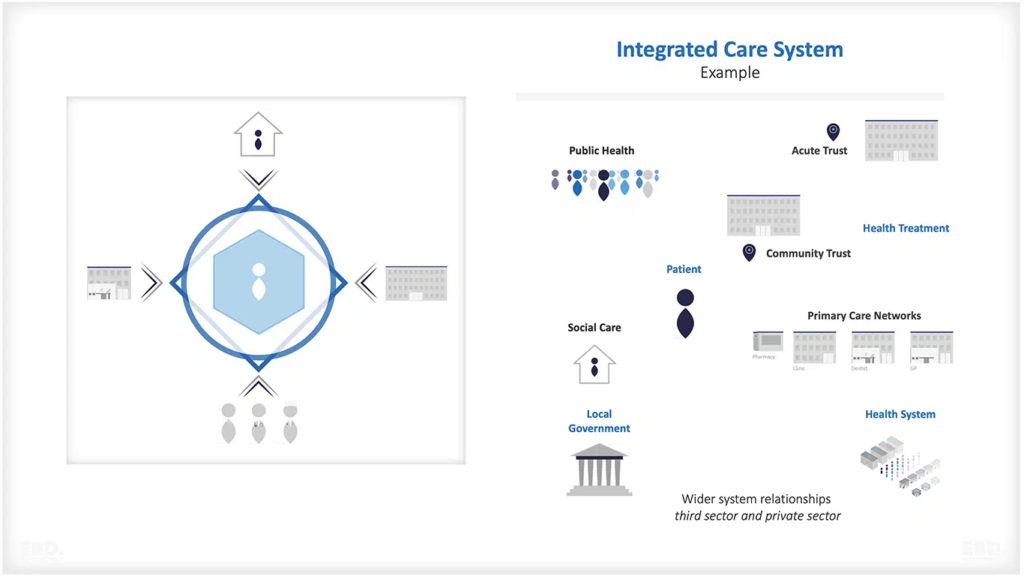
What is an Integrated Care System?
There are a variety of different models of integrated care, each with its own unique features. However, all models of integrated care share the same goal of improving the quality of care for patients/clients by reducing duplication of services and improving communication and coordination between different care providers.
The World Health Organisation defines integrated care:
“health services that are managed and delivered so that people receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease-management, rehabilitation and palliative care services, coordinated across the different levels and sites of care within and beyond the health sector, and according to their needs throughout the life course.” Integrated People-centered Health Services World Health Assembly (2016)
Integrated care can cover:
- Health promotion and disease prevention activities
- Vertical and horizontal integration for diagnosis, treatment and disease management services
- Rehabilitation and palliative care services
- Health and social care integration
Integrated care for individuals with complex health and care needs is often delivered through a care package approach, which is where a team of different health and social care professionals work together to provide coordinated care to a group of patients/clients with similar needs.
The care package approach is a key element of integrated care, as it ensures that patients/clients receive the right care from the right professionals at the right time. This approach also helps to improve communication and coordination between different care providers, as well as reducing duplication of services.
There is a huge variety of interventions which come under the umbrella of integrated care and the study by Baxter et al (2018) identified the following core types:
- joint assessment
- integrated care pathways
- shared / agreed referral criteria
- care coordination
- joint reviews / discharge
- integrated information technology and patient records
- new services
- multidisciplinary teams
- relocating / repurposing staff roles
- joint commissioning
- financial integration
- organisational integration
Of these, the most frequently cited were integrated care pathways and the use of multidisciplinary teams.
Different types of integrated care exist for low-income countries compared to high-income countries. Evidence from Mounier-Jack et al (2017) suggests that low-income countries tend to focus on the use of integrated care to improve the management of communicable diseases and to improve mental health. The focus of initiatives in high-income countries are interventions related to non-communicable diseases and ageing. High-income countries also focus on using integration to improve health system efficiency.
What is the evidence for integrated care systems?
It is not easy to navigate or summarise the evidence. The evidence landscape is complex and depends as much on the quality of the research as it does on the quality of the model of integration being studied. There are lots of case studies of good practice, and even where they have been well researched, they are all very different and results vary depending on culture, geography and the characteristics of the local health and care systems. There isn’t a simple model of integration which can be copied for spread and adoption.
However, there is evidence to suggest that there are benefits for:
- individuals and their families as access and timeliness of care is improved combined with a focus on outcomes that matter to patients
- local communities through improved population health and reduced health inequalities
- health systems through improved efficiency and better value from the use of resources
- the healthcare workforce as their experience of managing the workload improves and there is less wasted effort and duplication
The 5 strategies for successful integrated care?
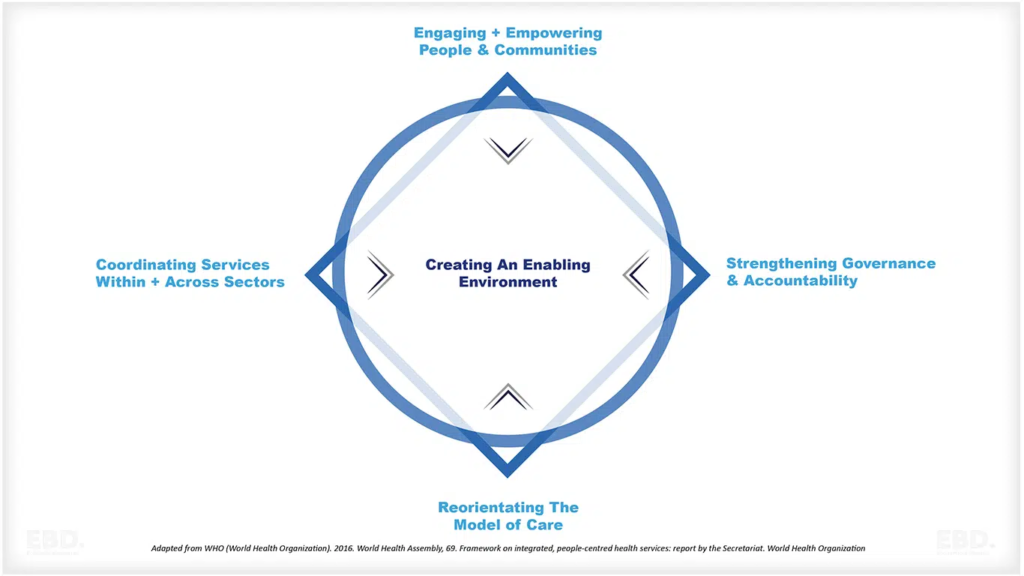
.The Framework on Integrated, People-Centered Health Services (IPCHS) (WHO 2016) proposes five strategies:
1. Empowering and engaging people and communities
Empowerment and engagement is important if efforts to improve population health and reduce health inequalities are to be effective. Typical policies include health literacy, education, shared decision-making, and community-based delivery models.
2. Strengthening governance and accountability
The key word here is stewardship with stakeholders working together to make decisions about the use of resources in a transparent and accountable way. Participatory governance and accountability to local populations enhance the likelihood of achieving health system goals through integrated care. Typical policies include patient charters, the use of patient experience performance metrics, and even community ownership models.
3. Reorienting the model of care
Integrated care is often used as a lever to improve prevention programmes and shift the focus of care from secondary to primary and community-based models often centred around particular geographies. This includes the use of digital health technologies to enable care to be delivered differently. New models of care embrace new models of working by health professional staff and collaboration between health and social care staff including multi-disciplinary and multi-professional teams (MDTs) and Case Coordinators.
4. Coordinating services within and across sectors
Coordination is a key feature of integrated care. Typical policy initiatives include care pathways, clinical networks, health navigators, case management, joint assessment and clear referral protocols. This should be reinforced through strategic purchasing for a population or a disease group or care pathway.
5. Creating an enabling environment through 6 approaches
Integrated care can be difficult to achieve without 6 key enabling strategies: These are
- transformational and distributed leadership and management, and a focus on continuous quality improvement,
- investment in digital infrastructure and associated information systems to enable the collecting and sharing of information in a clinical setting and to support population health management and chronic disease management.
- systems research and knowledge management to promote and enable evidence-informed practice
- workforce redesign and transformation supporting new skills and ways of working,
- reducing barriers through enabling regulatory frameworks, and
- funding and payment reforms which incentivise and reward integration.
10 examples of integrated care systems
There are many examples of integrated care systems around the world.
Here are some of the most well-known models that operate at a significant scale.
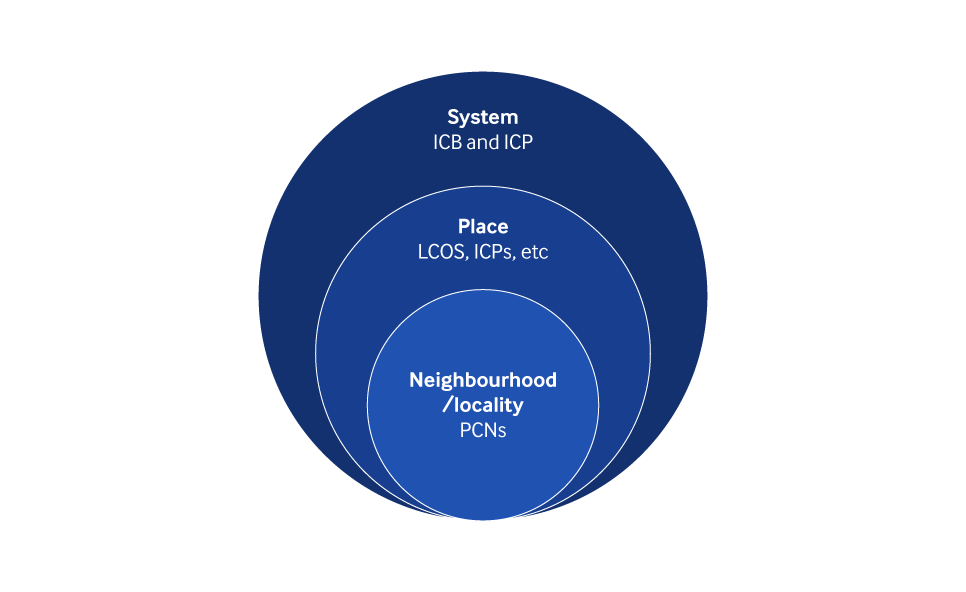
The NHS in England has been working towards this for some time with the introduction of 42 clinically led Integrated Care Systems (ICSs) effective July 2022.
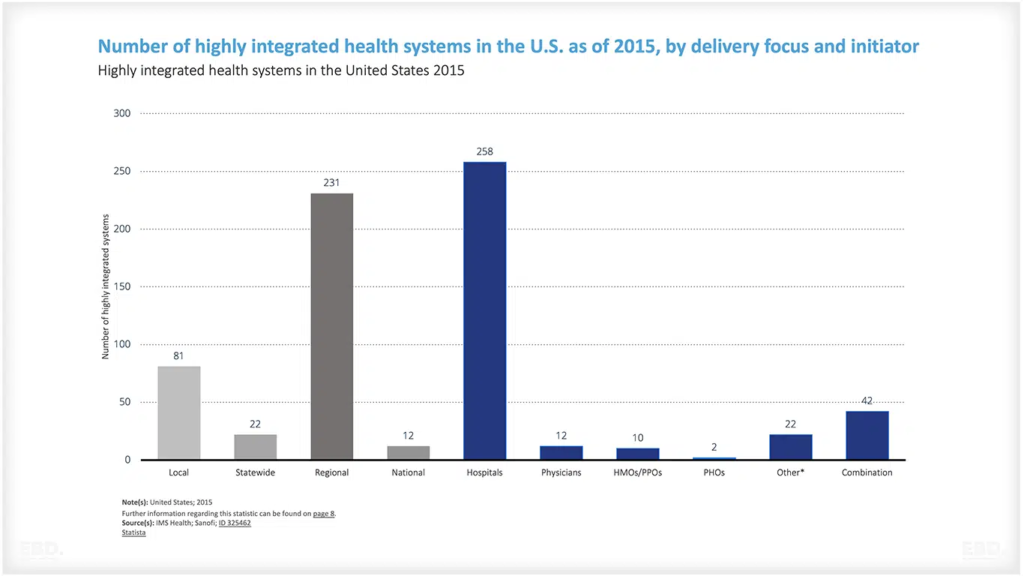
In the United States, the Veterans Health Administration has been working towards integration for over two decades and is often cited as an example of best practice.
The United States has also led the development of Accountable Care Organisations and Patient Centred Medical Homes both of which are designed to improve integrated care.
In Australia, there are several integrated care initiatives underway including the Primary Health Networks (PHNs) which were introduced in 2015 to deliver more coordinated care to patients with complex health needs.
In Canada, the Province of Alberta has established an Integrated Care Delivery System which includes several initiatives such as care coordination teams and Electronic Health Record (EHR) integration.
Ribera Salud is an integrated care system in Spain which is effective in reducing hospital admissions and improving the quality of life for patients with chronic conditions.
Gesundes Kinzigtal is a healthcare management company which operates a regional integrated care system in Germany and has responsibility for all the health outcomes in the region.
Regional Skane in Sweden is a successful integrated care system which integrated across health and social care and other sectors which drive population health. It connects social and medical care, public transport, economic development, social planning and the environment.
The Canterbury health system in New Zealand is also held up as an example of an integrated care system which is focused on population health, and care coordination.
In Ireland, the HSE has established four integrated care programmes for older people, children, prevention and mangeemnt of chronic disease, and patient flow.
Integrated Care Pathways
Integrated care relies on the effective use of care pathways or packages of care to ensure that patients receive the right care, at the right time, in the right place and from the right provider. A care pathway is a clinical road map which outlines the steps that need to be taken to manage a patient’s condition effectively.
Care pathways can be used to manage both acute and chronic conditions, and can help ensure that patients receive the right level of care, and do not receive unnecessary or duplicate tests or treatments. Care pathways are also a useful tool for managing complex cases which involve multiple providers and agencies.
The use of care pathways can help to improve communication between different care providers and can ensure that patients receive a coordinated and cohesive care experience.
What is the economic value of Integrated Care Systems?
Integrated care systems have the potential to add value to the economy by:
- improving health outcomes, healthy life expectancy, and the ability of individuals to contribute to society and the economy
- reducing waste and duplication in health service delivery, including at the interface between health and social care
- improving productivity of health resources and in particular enabling the health workforce to achieve the full potential of their skills and experience through collaboration and coordination
The evidence is complex due to the diverse nature of the topic, however, studies are consistently showing that well-designed systems and care pathways are demonstrating improvements in efficiency and outcomes compared with traditional siloed methods of health care provision.